


The Critical Role of Navigators in Improving Access to First-Line Precision Oncology Therapies for Advanced NSCLC
The treatment landscape for advanced non–small cell lung cancer (NSCLC) has undergone a paradigm shift with the advent of targeted therapies.1 Targeted therapies provide improved efficacy compared to chemotherapy alone or in combination with immunotherapy for patients with advanced NSCLC who harbor actionable genetic alterations.2,3 Key actionable biomarkers in NSCLC include ALK, RET, and ROS1 rearrangements; BRAF V600E, KRAS G12C, EGFR, ERBB2 (HER2), and MET exon 14 skipping mutations; and NTRK fusions.2 The ability to detect these mutations before first-line treatment can influence the choice of therapy, allowing for a more tailored approach that maximizes the likelihood of treatment success while minimizing unnecessary exposure to ineffective treatments.4,5
Comprehensive genomic profiling allows for the complete assessment of all actionable alterations in a single test, enabling faster turnaround times and reduced time from diagnosis to first-line therapy compared with sequential single-gene tests.6-8 However, despite the improved efficacy of targeted therapy compared to chemotherapy alone or in combination with immunotherapy in patients with advanced NSCLC who harbor actionable genetic alterations, only a portion of eligible patients with advanced NSCLC receive appropriate precision oncology therapies. Barriers to molecular testing contribute to missed opportunities for treatment with targeted therapies.9
Patient and tissue navigators are increasingly recognized for their roles in improving health-care delivery.10 Tissue navigators are professionals in the pathology laboratory who serve as liaisons between patients, pathologists, treating physicians, and external laboratories.11 Their importance has become increasingly evident with the approval of precision medicine therapies.11 Patient navigators are trained professionals who assist patients in navigating the complexities of health-care systems, particularly in oncology and chronic disease management.12 Both patient and tissue navigators can have an impact and may work together to collectively benefit patients with NSCLC. This article explores the potential role of patient and tissue navigators in overcoming barriers to timely comprehensive molecular profiling in patients with advanced NSCLC (Figure 1).
Figure 1. Potential Tissue and Patient Navigator Roles in Overcoming Barriers Along the Precision Oncology Pathway9
Biopsy referral
Biospecimen collection
Biospecimen evaluation/ pathology
Biomarker test ordering
Biomarker testing performance
Test result reporting
Treatment decision
Benefits of Comprehensive Genomic Profiling in Advanced NSCLC Before First-Line Treatment
By allowing the simultaneous identification of actionable mutations,13 comprehensive genomic profiling is a cost-effective strategy to increase the percentage of eligible patients with NSCLC who receive biomarker-driven first-line therapies.14 Recent evidence suggests that the benefits of comprehensive molecular testing may be greater if conducted before first-line treatment.5 Compared with small panel testing, comprehensive molecular profiling before first-line treatment increases the rates of appropriate precision therapy and improves overall survival for patients with advanced NSCLC.15,16 In a recent real-world study comparing comprehensive genomic profiling with small panel testing in advanced NSCLC, patients who underwent comprehensive genomic profiling before first-line treatment had better detection of actionable genetic alterations, a higher likelihood of receiving matched therapies, and improved survival rates compared with patients who underwent small panel testing.16
“Establishing the molecular profile of patients with NSCLC is one of the most important steps to properly manage a patient with newly diagnosed NSCLC,” emphasized Tarek Mekhail, MD, Medical Director of the Thoracic Cancer program at AdventHealth Cancer Institute. “Not only does it guide treatment decisions, but it also informs us about disease behavior, staging, and prognosis. There is clear evidence that patient outcomes are improved when regimens are chosen based on molecular profiling rather than by histology alone.”
Establishing the molecular profile of patients with NSCLC is one of the most important steps to properly manage a patient with newly diagnosed NSCLC. … There is clear evidence that patient outcomes are improved when regimens are chosen based on molecular profiling rather than by histology alone. Tarek Mekhail, MD
A real-world study comparing timely (results available before first-line treatment) to delayed (results available after first-line treatment) comprehensive genomic profiling showed that timely testing increased the use of matched targeted therapies (17% vs 2.8%) and precision immune checkpoint inhibitors (18% vs 3.9%) in patients with advanced NSCLC.5 Timely comprehensive molecular profiling also reduced the use of ineffective immune checkpoint inhibitors among patients with ALK/EGFR/RET/ROS1-positive tumors, resulting in substantial cost savings.5 Moreover, patients who underwent comprehensive molecular testing before first-line treatment experienced longer real-world time to therapy discontinuation compared to those with delayed testing results.5
Barriers to Upfront Comprehensive Genomic Profiling in Advanced NSCLC
Despite the benefits of comprehensive molecular profiling when determining first-line treatment for patients with advanced NSCLC, there are barriers to its widespread adoption (Figure 1). Real-world data demonstrate that less than 50% of patients with metastatic NSCLC undergo next-generation sequencing (NGS) before first-line treatment, suggesting the underuse of comprehensive molecular profiling to guide first-line treatment decisions.8 A retrospective study of 814 patients with advanced NSCLC treated in community settings demonstrated that only 8% of patients underwent NGS, suggesting the presence of several challenges in implementing comprehensive molecular profiling in the community oncology setting.17 Another real-world study of over 500,000 patients with NSCLC in the United States showed that only 36% of eligible patients with advanced NSCLC receive appropriate precision oncology therapies and that barriers in biomarker testing account for 31% of missed opportunities for treatment with targeted therapies in this patient population.9
“A primary barrier in preventing eligible NSCLC patients from receiving targeted therapy is a lack of pathology programs with internal staffing to triage cases and ensure the tissue is handled correctly and submitted for appropriate biomarker studies,” explained Rosanna Lapham, MD, pathologist at Spartanburg Regional Healthcare System. “To overcome these barriers, institutions need established policies and procedures regarding tissue handling. It is essential to have dedicated, trained, centralized lab associates to perform these tasks and not outsource to clinical oncology staff.”
A primary barrier in preventing eligible NSCLC patients from receiving targeted therapy is a lack of pathology programs with internal staffing to triage cases and ensure the tissue is handled correctly and submitted for appropriate biomarker studies. Rosanna Lapham, MD
Obtaining adequate tissue samples for comprehensive profiling is a common issue. In a study involving 814 patients with advanced NSCLC, 13% had insufficient tissue for genotyping.17 Another study showed that 17% of comprehensive molecular profiling orders were canceled because of tissue insufficiency when single-gene testing was performed first.18
Although Dr. Mekhail acknowledged that insufficient tissue is a common issue, he noted that adequacy of tissue samples should not hinder molecular testing for clinical decision-making. “NGS can now be performed on minute tissue samples, including fine-needle biopsies. We now also have the ability to perform comprehensive NGS on circulating DNA.”
Economic factors may also contribute to the limited implementation of comprehensive molecular profiling. A survey of 143 community medical oncologists identified insurance coverage and reimbursement as the biggest obstacles to using NGS profiling.19 The cost of comprehensive genomic profiling to patients was the third most significant barrier reported by the surveyed oncologists.19 Logistical challenges in tissue acquisition and processing, and lack of standardization in testing methodologies and reporting also pose challenges that may limit the widespread adoption of comprehensive molecular profiling before first-line treatment for patients with advanced NSCLC.20-23 Additional barriers that hinder eligible patients from receiving appropriate targeted therapies include gaps in biopsy referral, biospecimen collection, and biospecimen evaluation.9
The use of multidisciplinary tumor boards has been shown to reduce the time from diagnosis to treatment, increase adherence to treatment guidelines, and increase the overall patient survival rate in patients with NSCLC.24-27 However, the lack of integration among multidisciplinary team members, such as oncologists, pathologists, and geneticists, may exacerbate delays in the implementation of molecular testing and initiation of appropriate precision oncology treatments.28
Role of Tissue Navigators in Improving Access to Precision Oncology Therapies for Advanced NSCLC
Ensuring sufficient sample quantity and quality is particularly important for comprehensive molecular profiling because most NGS platforms require a sample size of at least 25 mm² tumor surface area and ≥ 20% tumor content per sample to detect mutations accurately.29,30 Evidence suggests that tissue navigators can help increase the success rate of comprehensive genomic profiling. In a recent article, Tavora et al reported that implementation of a proactive approach involving a tissue navigator in their practice led to an increase from approximately 25% to over 60% in the number of patients with advanced NSCLC who underwent molecular testing.11
“Biomarker tissue navigators contribute to the timely initiation of the right first-line treatment for patients with NSCLC by serving as a conduit between pathology and oncology, ensuring the right test is ordered on the right patient at the right time,” emphasized Amanda Hanson, Director of Precision Medicine at Spartanburg Regional Healthcare System. “Each patient is independently triaged and not automatically reflexed. Biomarker tissue navigators consider each case and the limited tissue nature of NSCLC cases, ensuring the optimized specimen is sent for appropriate testing and preserving as much precious tissue as possible.”
Biomarker tissue navigators contribute to the timely initiation of the right first-line treatment for patients with NSCLC by serving as a conduit between pathology and oncology, ensuring the right test is ordered on the right patient at the right time. Amanda Hanson
Tissue navigators are well positioned to track tissue samples from the point of biopsy to ensure they are adequate for comprehensive molecular profiling and that there are no delays or errors that would negatively affect treatment.31,32 By flagging insufficient tissues and reporting reasons for insufficiency, tissue navigators can help establish consistent communication feedback loops between pathologists and clinical care teams regarding common barriers to molecular testing.31
At Spartanburg Regional Healthcare System, the implementation of tissue navigators has led to several measurable improvements, as Dr. Lapham noted: “Using the precision pathology model and having dedicated staff, our biomarker tissue navigators improved efficiency through reduction in send-out testing turnaround times to under 24 hours, reduction in Quantity Not Sufficient results through optimal block selection, increased clinician efficiency by reducing the burden on pathologists, and better tissue preservation by ensuring appropriate initial testing and reducing multiple cuts into the block.”
Tissue navigators may help enhance effective and timely molecular testing for patients with advanced NSCLC by streamlining tissue acquisition and processing workflows and facilitating test ordering.11 These can be achieved by ensuring efficient identification of cases requiring molecular testing, timely acquisition of patient consent, optimal utilization of limited tissue resources, and selection of appropriate tissue blocks for molecular testing.11 Tissue navigators also communicate results to treating physicians and liaise between pathologists and treating physicians to minimize delays in test ordering and treatment decisions.11
“We’ve transformed our workflow so that oncology providers are no longer directly ordering molecular testing through various portals but rather utilizing the EMR to place the order that goes to the biomarker tissue navigators,” explained Mrs. Hanson. “This removes the responsibility of clinical staff to find time to order and retrieve results from multiple portals and allows them to focus on patient care. Our biomarker tissue navigators ensure the results are properly uploaded to the EMR and follow up on missing results.”
In addition, tissue navigators play a crucial role in obtaining informed consent from patients before submitting tissue blocks to external laboratories for molecular testing.11 This process entails educating patients about molecular testing and its role in clinical decision-making, addressing the concerns of patients and their families, and facilitating administration tasks related to tissue shipment.11 Therefore, implementation of tissue navigators can alleviate the pathologist’s workload, enabling pathologists to focus on their diagnostic duties.11
As liaisons between the pathology department and the care team, tissue navigators ensure that treating physicians remain up-to-date with molecular testing results and flag actionable information that is relevant to treatment decisions or cases where further testing may be required.11 They are also well positioned to help the multidisciplinary team navigate the complex landscape of available biomarker tests, patient eligibility, and molecular testing results, which could reduce delays in test ordering and treatment initiation.11
Tissue navigators may also help address economic barriers to comprehensive molecular profiling. By ensuring that tissue samples are collected and submitted correctly, navigators can prevent delays and additional costs associated with repeat testing. For example, in a study involving comprehensive genomic profiling of patients with lung cancer, proper sample handling led to a high success rate for obtaining sufficient DNA for NGS, even for fine-needle aspirates.33 Furthermore, as pathology laboratory experts, tissue navigators can optimize sample selection and fixation protocols to ensure high-quality DNA extraction, which reduces sequencing errors and costs.34 In addition, tissue navigators are well positioned to advocate for policy changes that promote universal coverage of NGS for all patients, regardless of their insurance status. A study has shown that patients with Medicare or underinsured status are less likely to receive genetic sequencing, highlighting the need for broader coverage.35
Role of Patient Navigators in Improving Access to Precision Oncology Therapies for Advanced NSCLC
Patient navigators can be health-care professionals such as nurses (often called nurse navigators), allied health professionals such as social workers or health educators, or trained laypersons.36 Nurse navigators typically have clinical expertise in addition to navigation skills and focus on various clinical and support services, whereas lay navigators focus primarily on coordination and support by linking patients to the appropriate health-care providers.36 Patient navigators serve as liaisons between patients, physicians, and other health-care providers, coordinating and streamlining various aspects of multidisciplinary care, including molecular testing.31,37
Patient navigators help schedule patients for biopsy for diagnosis and cancer staging, consolidate reports, upload reports in electronic medical record systems, follow up on test results, facilitate multidisciplinary discussions, communicate testing findings, and ensure that patients are informed and supported throughout their treatment journey.38 Effective recordkeeping, including the use of electronic medical records with integrated alerts for requests for molecular testing and availability of molecular testing results, can help streamline communication and decision-making processes related to molecular testing in NSCLC.31 In a study of the effects of implementation of nurse navigators on the rates of molecular testing in patients with NSCLC, molecular testing rates rose from 62% to 91% following the integration of a nurse navigator into the care process.39
“Our patient navigators keep track of all patients scheduled to see medical oncology,” explained Dr. Mekhail. “Before the date of the visit, they ensure that molecular testing has been ordered and completed, or is at least in progress.”
Our patient navigators keep track of all patients scheduled to see medical oncology. Before the date of the visit, they ensure that molecular testing has been ordered and completed, or is at least in progress. Tarek Mekhail, MD
Furthermore, evidence suggests that patient navigators can reduce the time to treatment initiation, which is a key determinant of patient outcomes.40 For instance, the implementation of a thoracic multidisciplinary clinic involving a nurse navigator has been associated with reduced time to treatment initiation and a greater concordance with clinical pathways for patients with advanced NSCLC.41 A retrospective cohort study compared survival outcomes in patients with NSCLC before and after implementation of OnkoNetwork (control and intervention cohorts, respectively), a patient navigation program.42 The study showed that implementation of patient navigation led to a significant survival benefit for patients with NSCLC, with a hazard ratio of 0.63 (P = .039), indicating a 37% reduction in the risk of death compared to the control cohort (Figure 2).42
Figure 2. Effect of Patient Navigation on Weighted Overall Survival of Patients With NSCLC42
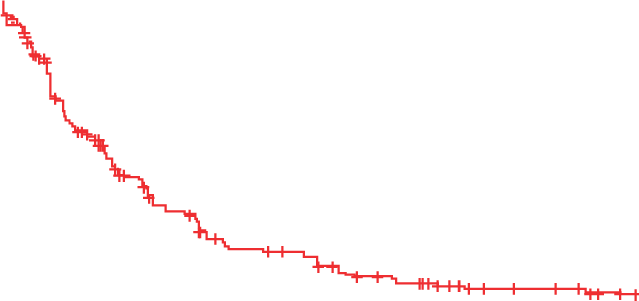

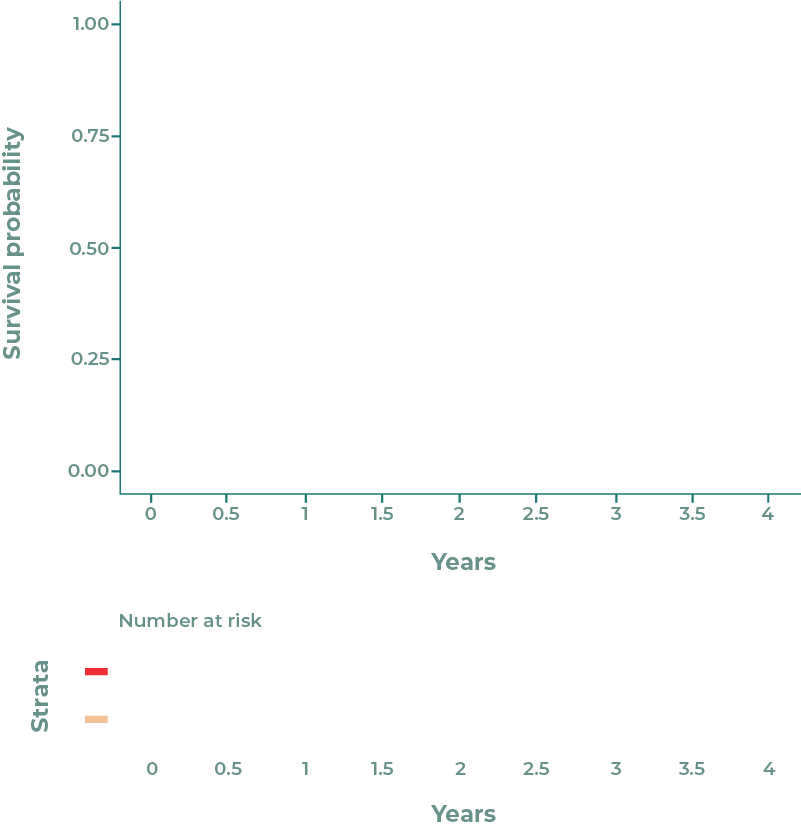
Adapted from Pitter et al.42 Licensed under the Creative Commons Attribution 4.0 License: http://creativecommons.org/licenses/by/4.0/.
Abbreviations: NSCLC = non–small cell lung cancer.
The presence of patient navigators may improve patient satisfaction and engagement in their care. In a systematic review of 59 studies involving patients with cancer, 71% of studies showed significant improvements in treatment adherence and 87% (13 out of the 15) of the studies reported high rates of patient satisfaction with the implementation of patient navigation programs.40 In addition, 81% of studies indicated a positive impact of patient navigation on quality care indicators.40 Furthermore, a national quality survey on care coordination for advanced NSCLC demonstrated that the presence of patient navigators improved shared decision-making and patient experience along the lung cancer care continuum.43 Programs with patient navigators showed higher mean decision-making scores than programs without navigators.43
Patient navigation is particularly beneficial for disadvantaged populations.40 In a meta-analysis of 37 studies on cancer treatment in disadvantaged groups, 28 (76%) had positive conclusions regarding the role of patient navigators during cancer treatment.40 For treatment initiation, 8 out of 16 studies that found improvements in cancer care with navigation were focused on disadvantaged patients. These studies showed navigation reduced the time to treatment initiation for underserved groups. For treatment adherence, 8 out of 12 studies that demonstrated enhanced treatment adherence rates were done in disadvantaged populations.40 A meta-analysis of data from nine centers comparing patient navigation with usual care showed that the benefits of patient navigation in terms of cancer treatment initiation were greatest at centers with delays in follow-up, supporting the adoption of navigation programs in underserved populations.44
Patient navigators may also help address economic barriers to comprehensive molecular profiling. One of the primary functions of patient navigators is to assist patients in navigating the complexities of health insurance and out-of-pocket expenses associated with molecular profiling.45 Research indicates that financial concerns are among the most significant barriers that patients encounter.46 Patient navigators provide instrumental support by helping patients understand their insurance benefits, identify potential coverage for NGS, and explore financial assistance programs that may alleviate the costs associated with testing.47 This support is particularly vital in populations that may have limited financial resources or face economic disparities, as it can lead to increased access to essential diagnostic tools that inform treatment decisions.
Conclusions
The integration of comprehensive genomic profiling into clinical workflows for advanced NSCLC has the potential to improve patient outcomes by informing appropriate biomarker-driven treatment decisions.13-16 However, realizing this potential requires overcoming several barriers, including limited tissue availability, delays in test ordering and analysis, and inadequate integration among multidisciplinary team members.20,22,23,28 The roles of patient and tissue navigators are pivotal in addressing these challenges and in ensuring timely and efficient molecular testing.31,37,39 By coordinating care, facilitating communication, and ensuring the efficient use of tissue samples, navigators help ensure that eligible patients receive timely and appropriate targeted therapies.41
The roles of tissue and patient navigators are complementary; hence, integrating both tissue and patient navigators is crucial for optimizing the molecular testing process and patient care in institutions treating advanced NSCLC. Tissue navigators focus on the technical aspects of sample management and testing, increasing the number of patients with NSCLC who undergo molecular profiling.11 Patient navigators, on the other hand, guide patients through the complexities of their cancer journey and help address barriers to care, improving treatment initiation and adherence.37,40 Together, these roles create a more efficient and patient-centered approach to precision oncology, potentially leading to improved outcomes and patient satisfaction.
According to Mrs. Hanson, the most significant barrier for health-care institutions looking to implement tissue navigation programs is justifying employing dedicated staff in what is considered a non-revenue-generating role. “To help overcome this barrier, it is critical to recognize that these tasks are already being done, but sporadically, by many personnel that otherwise have patient care responsibilities,” she said. By centralizing these tasks under dedicated navigators, institutions can ensure more timely molecular testing, which directly impacts patient care. Expanded and timely adoption of comprehensive molecular testing can lead to faster diagnosis and treatment initiation, reducing the time patients spend waiting for critical therapy decisions.6-8
Although Dr. Mekhail acknowledges the financial barriers to implementing patient navigation programs, he believes that the value navigators provide is worth the costs. “They significantly improve patient care, help coordinate multispeciality visits, ensure orders are performed in a timely fashion, and help avoid unnecessary visits,” he said. “All this ultimately leads to better outcomes and significantly improves patient satisfaction.”
[Navigators] significantly improve patient care, help coordinate multispeciality visits, ensure orders are performed in a timely fashion, and help avoid unnecessary visits. All this ultimately leads to better outcomes and significantly improves patient satisfaction. Tarek Mekhail, MD
Dr. Lapham offers a practical approach to program implementation: “Grants are available to start a program. Then by tracking key performance indicators along with patient and provider satisfaction, an institution can show a strong patient care return on investment to continue and even expand the program.”
For community oncologists looking to improve their molecular testing practices, Dr. Lapham recommends “working with hospital administration to develop and fund standardized precision medicine/precision pathology programs and employ dedicated biomarker tissue navigators with a laboratory background to handle all the details of sending out molecular testing.”
Continuing efforts for timely and efficient comprehensive molecular testing to determine the best first-line treatment, supported by robust navigation strategies, are key to ensuring that more patients benefit from advances in precision oncology treatment, ultimately leading to improved survival and quality of life for patients with advanced NSCLC.
Disclosures
Mrs. Hanson reported receiving honoraria from AstraZeneca.
Dr. Lapham reported receiving honoraria from Lilly.
Dr. Mekhail reported receiving honoraria from Genentech/Roche, Lilly, Bristol Myers Squibb, Merck, AstraZeneca, Amgen, Coherus BioSciences, and Daiichi Sankyo; and speakers’ bureau participation with Genentech/Roche, Lilly, Bristol Myers Squibb, and Merck.
References
- Yuan M, Huang LL, Chen JH, et al: The emerging treatment landscape of targeted therapy in non-small-cell lung cancer. Signal Transduct Target Ther 4:61, 2019
- Li S, de Camargo Correia GS, Wang J, et al: Emerging targeted therapies in advanced non-small-cell lung cancer. Cancers (Basel) 15, 2023
- Yang G, Yang Y, Liu R, et al: First-line immunotherapy or angiogenesis inhibitor combined with chemotherapy for advanced non-small cell lung cancer with EGFR exon 20 insertions: Real-world evidence from China. Cancer Med 12:335-344, 2023
- Fox AH, Nishino M, Osarogiagbon RU, et al: Acquiring tissue for advanced lung cancer diagnosis and comprehensive biomarker testing: A National Lung Cancer Roundtable best-practice guide. CA Cancer J Clin 73:358-375, 2023
- Yorio J, Lofgren KT, Lee JK, et al: Association of timely comprehensive genomic profiling with precision oncology treatment use and patient outcomes in advanced non-small-cell lung cancer. JCO Precis Oncol 8:e2300292, 2024
- Zheng Y, Vioix H, Liu FX, et al: Diagnostic and economic value of biomarker testing for targetable mutations in non-small-cell lung cancer: a literature review. Future Oncol 18:505-518, 2022
- Pennell NA, Mutebi A, Zhou ZY, et al: Economic impact of next-generation sequencing versus single-gene testing to detect genomic alterations in metastatic non-small-cell lung cancer using a decision analytic model. JCO Precis Oncol 3:1-9, 2019
- Robert NJ, Espirito JL, Chen L, et al: Biomarker testing and tissue journey among patients with metastatic non-small cell lung cancer receiving first-line therapy in The US Oncology Network. Lung Cancer 166:197-204, 2022
- Sadik H, Pritchard D, Keeling DM, et al: Impact of clinical practice gaps on the implementation of personalized medicine in advanced non-small-cell lung cancer. JCO Precis Oncol 6:e2200246, 2022
- Kokorelias KM, Shiers-Hanley JE, Rios J, et al: Factors influencing the implementation of patient navigation programs for adults with complex needs: a scoping review of the literature. Health Serv Insights 14:11786329211033267, 2021
- Tavora F, de Sousa JC: Tissue navigator, an important position in the Pathology laboratory in the Precision Medicine era. ESMO Open 8:101827, 2023
- Clark JA, Parker VA, Battaglia TA, et al: Patterns of task and network actions performed by navigators to facilitate cancer care. Health Care Manage Rev 39:90-101, 2014
- Singh AP, Shum E, Rajdev L, et al: Impact and diagnostic gaps of comprehensive genomic profiling in real-world clinical practice. Cancers (Basel) 12, 2020
- Zou D, Ye W, Hess LM, et al: Diagnostic value and cost-effectiveness of next-generation sequencing-based testing for treatment of patients with advanced/metastatic non-squamous non-small-cell lung cancer in the United States. J Mol Diagn 24:901-914, 2022
- Meng R, Dowdell AK, Vita A, et al: Clinical impact for advanced non-small-cell lung cancer patients tested using comprehensive genomic profiling at a large USA health care system. ESMO Real World Data and Digital Oncology 5:100057, 2024
- Wallenta Law J, Bapat B, Sweetnam C, et al: Real-world impact of comprehensive genomic profiling on biomarker detection, receipt of therapy, and clinical outcomes in advanced non-small cell lung cancer. JCO Precis Oncol 8:e2400075, 2024
- Gutierrez ME, Choi K, Lanman RB, et al: Genomic profiling of advanced non-small cell lung cancer in community settings: gaps and ppportunities. Clin Lung Cancer 18:651-659, 2017
- Nesline MK, Subbiah V, Previs RA, et al: The impact of prior single-gene testing on comprehensive genomic profiling results for patients with non-small cell lung cancer. Oncol Ther 12:329-343, 2024
- Marshall J, Buettner A, Lankford ML, et al: Comprehensive tumor genomic testing in the community oncology setting in the United States. Journal of Clinical Oncology 36:e24304-e24304, 2018
- Morris SM, Subramanian J, Gel ES, et al: Performance of next-generation sequencing on small tumor specimens and/or low tumor content samples using a commercially available platform. PLoS One 13:e0196556, 2018
- Deverka PA, Kaufman D, McGuire AL: Overcoming the reimbursement barriers for clinical sequencing. JAMA 312:1857-8, 2014
- Maani N, Panabaker K, McCuaig JM, et al: Incidental findings from cancer next generation sequencing panels. NPJ Genom Med 6:63, 2021
- Malapelle U, Leighl N, Addeo A, et al: Recommendations for reporting tissue and circulating tumour (ct)DNA next-generation sequencing results in non-small cell lung cancer. Br J Cancer 131:212-219, 2024
- Senter J, Hooker C, Lang M, et al: Thoracic multidisciplinary clinic improves survival in patients with lung cancer. International Journal of Radiation Oncology, Biology, Physics 96:S134, 2016
- Freeman RK, Van Woerkom JM, Vyverberg A, et al: The effect of a multidisciplinary thoracic malignancy conference on the treatment of patients with lung cancer. Eur J Cardiothorac Surg 38:1-5, 2010
- Huang B, Chen Q, Allison D, et al: Molecular tumor board review and improved overall survival in non-small-cell lung cancer. JCO Precis Oncol 5, 2021
- Ray MA, Faris NR, Fehnel C, et al: Survival impact of an enhanced multidisciplinary thoracic oncology conference in a regional community health care system. JTO Clin Res Rep 2:100203, 2021
- Chamala S, Maness HTD, Brown L, et al: Building a precision oncology workforce by multidisciplinary and case-based learning. BMC Med Educ 21:75, 2021
- Tomlins SA, Hovelson DH, Suga JM, et al: Real-world performance of a comprehensive genomic profiling test optimized for small tumor samples. JCO Precis Oncol 5, 2021
- Smits AJ, Kummer JA, de Bruin PC, et al: The estimation of tumor cell percentage for molecular testing by pathologists is not accurate. Mod Pathol 27:168-74, 2014
- Fintelmann FJ, Martin NA, Tahir I, et al: Optimizing molecular testing of lung cancer needle biopsy specimens: potential solutions from an interdisciplinary qualitative study. Respir Res 24:17, 2023
- Gregg JP, Li T, Yoneda KY: Molecular testing strategies in non-small cell lung cancer: optimizing the diagnostic journey. Transl Lung Cancer Res 8:286-301, 2019
- Yang SR, Lin CY, Stehr H, et al: Comprehensive genomic profiling of malignant effusions in patients with metastatic lung adenocarcinoma. J Mol Diagn 20:184-194, 2018
- Berrino E, Bellomo SE, Chesta A, et al: Alternative tissue fixation protocols dramatically reduce the impact of DNA artifacts, unraveling the interpretation of clinical comprehensive genomic profiling. Lab Invest 104:100280, 2024
- Bade R, Banaszak LG, Osman F, et al: Neighborhood disadvantage, insurance status, and molecular profiling of patients with acute myeloid leukemia. Leuk Res 131:107326, 2023
- Meade CD, Wells KJ, Arevalo M, et al: Lay navigator model for impacting cancer health disparities. J Cancer Educ 29:449-57, 2014
- Wells KJ, Battaglia TA, Dudley DJ, et al: Patient navigation: state of the art or is it science? Cancer 113:1999-2010, 2008
- Doerfler-Evans RE: Shifting paradigms continued-the emergence and the role of nurse navigator. J Thorac Dis 8:S498-500, 2016
- Zibrik K, Laskin J, Ho C: Integration of a nurse navigator into the triage process for patients with non-small-cell lung cancer: creating systematic improvements in patient care. Curr Oncol 23:e280-3, 2016
- Chen M, Wu VS, Falk D, et al: Patient navigation in cancer treatment: a systematic review. Curr Oncol Rep 26:504-537, 2024
- Friedman EL, Kruklitis RJ, Patson BJ, et al: Effectiveness of a thoracic multidisciplinary clinic in the treatment of stage III non-small-cell lung cancer. J Multidiscip Healthc 9:267-74, 2016
- Pitter JG, Moizs M, Ezer ES, et al: Improved survival of non-small cell lung cancer patients after introducing patient navigation: A retrospective cohort study with propensity score weighted historic control. PLoS One 17:e0276719, 2022
- Aversano J, Boehmer LM, Spira A: Improving cancer care delivery: learnings for oncology nurses and patient navigation from a national quality survey. J Adv Pract Oncol 13:484-493, 2022
- Freund KM, Battaglia TA, Calhoun E, et al: Impact of patient navigation on timely cancer care: the Patient Navigation Research Program. J Natl Cancer Inst 106:dju115, 2014
- Doherty MJ, Thom B, Gany F: Evidence of the feasibility and preliminary efficacy of oncology financial navigation: a scoping review. Cancer Epidemiol Biomarkers Prev 30:1778-1784, 2021
- Paskett ED, Harrop JP, Wells KJ: Patient navigation: an update on the state of the science. CA Cancer J Clin 61:237-49, 2011
- Rodday AM, Parsons SK, Snyder F, et al: Impact of patient navigation in eliminating economic disparities in cancer care. Cancer 121:4025-34, 2015
VV-OTHR-US-DEL-3805 © 2024 Lilly USA, LLC. All rights reserved.
Disclaimer
Sponsored content is not written by and does not necessarily reflect the views of ASCO or The ASCO Post editorial staff. It is authored by Harborside Studio writers or independent medical writers approved by Harborside Studio. Harborside Studio's sponsored content is held to editorial standards expected in The ASCO Post with the intent to provide valuable information to The ASCO Post readers. Interviewed experts receive no remuneration for their comments. The mention of any company, product, service, or therapy does not constitute an endorsement of any kind by ASCO. ASCO assumes no responsibility for any injury or damage arising out of or related to use of the sponsored content or any errors or omissions. Lilly Medical Affairs provided early input on the topic and reviewed the final content for scientific accuracy. This content was produced with funding support from Lilly Medical Affairs and is intended for U.S. health-care professionals only.