




Mantle cell lymphoma (MCL) is a rare, aggressive subtype of B-cell lymphoma, accounting for less than 6% of all B-cell non-Hodgkin lymphomas. The presence of high-risk disease features can contribute to a worse prognosis.1 Unfortunately, the majority of patients with MCL are either refractory to treatment or develop resistance to standard first- and second-line therapy, including Bruton’s tyrosine kinase (BTK) inhibitors. Many patients who are refractory to or relapse after treatment with a covalent BTK inhibitor have a poor prognosis and thus represent a high-risk clinical group for which effective therapy has been lacking. This treatment gap highlights the continuing unmet need for novel therapies for patients with relapsed or refractory MCL, particularly in the third-line setting and beyond following progression on a covalent BTK inhibitor.
For newly diagnosed patients with MCL, first-line treatment depends on their clinical status. Younger, fit patients can receive high-dose induction chemotherapy followed by consolidation with autologous stem cell transplant (ASCT) and rituximab maintenance therapy. Older patients with comorbidities may receive less intensive chemotherapy, with maintenance rituximab.
Relapsed/refractory MCL is often characterized by treatment resistance and serial relapses. BTK inhibitors constitute a mainstay of therapy for relapsed/refractory MCL and have improved outcomes for many patients. Ibrutinib was the first BTK inhibitor approved for treatment of relapsed/refractory MCL. It received accelerated approval based on the results of a phase II trial that demonstrated an improved overall response rate in previously treated patients.2 Although ibrutinib therapy can result in high response rates, resistance mutations limit its long-term use. Primary ibrutinib resistance occurs in 10% to 35% of patients and acquired resistance in up to 40%; such resistance is associated with a poor prognosis, with a median overall survival of 6 to 10 months.1,3 The most common adverse events seen in ibrutinib-treated patients with B-cell malignancies (including MCL) were thrombocytopenia, diarrhea, fatigue, musculoskeletal pain, neutropenia, rash, anemia, infections, cardiac arrhythmias, and bruising.4 In April 2023, the pharmaceutical manufacturer of ibrutinib voluntarily withdrew this indication in relapsed MCL after the confirmatory phase III SHINE trial failed to show a significant overall survival benefit.5,6
Non–BTK inhibitor regimens, including those involving salvage chemoimmunotherapy (eg, bendamustine, lenalidomide, rituximab, venetoclax, bortezomib), can be useful as second-line or later therapy in certain circumstances, but their efficacy is limited and resistance often develops.7 For patients who experience disease progression following second-line therapy, recommended approved third-line options are limited to the noncovalent BTK inhibitor pirtobrutinib and the chimeric antigen receptor (CAR) T-cell therapy brexucabtagene autoleucel; enrollment in a clinical trial is also an option.
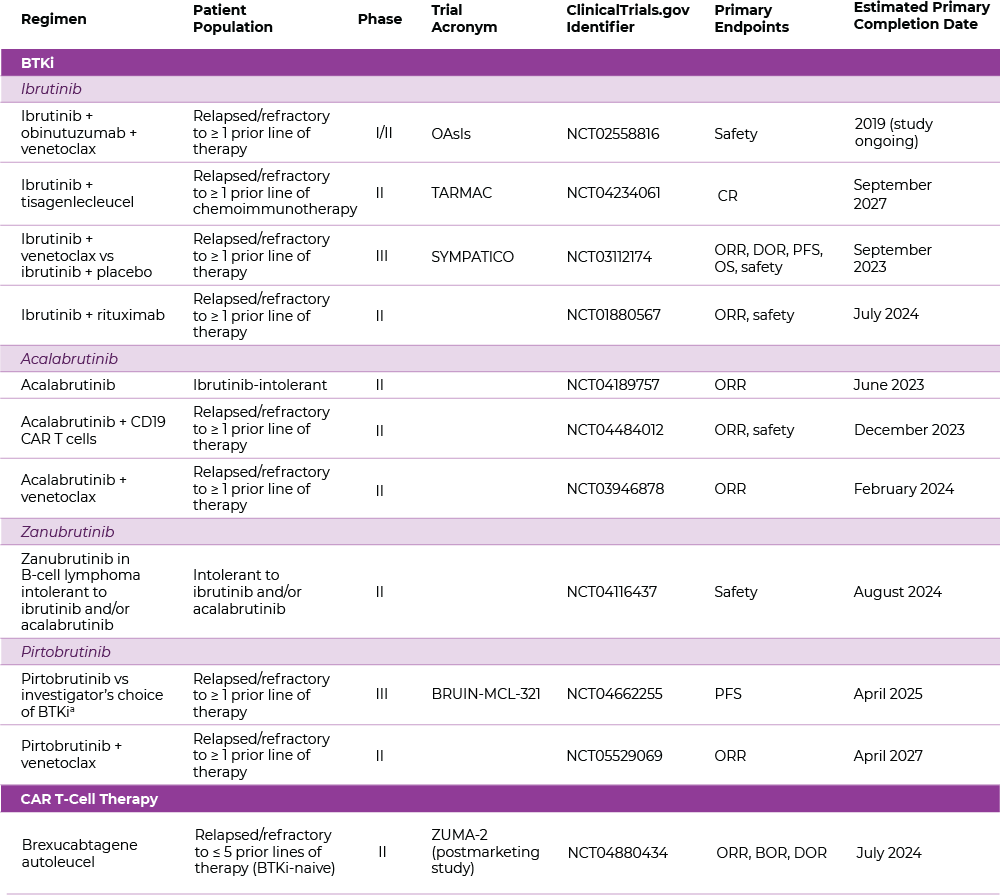
Following the approval of ibrutinib, next-generation BTK inhibitors were identified and evaluated for treatment of relapsed/refractory MCL to improve efficacy and reduce treatment-related toxicity. These agents include the covalent inhibitors acalabrutinib and zanubrutinib as well as the noncovalent BTK inhibitor pirtobrutinib.8 Regimens employing these agents, as well as other novel approaches such as CAR T-cell therapy, are continuing to be evaluated for relapsed/refractory MCL in phase II or III clinical trials (Table 1).
Acalabrutinib is a covalent, irreversible BTK inhibitor that is more potent and more selective for BTK than ibrutinib, with a shorter half-life. In a phase II trial in relapsed/refractory MCL (patients had a median of two prior lines of therapy), acalabrutinib therapy resulted in an overall response rate of 81.0% (40% complete response rate) and a 12-month median progression-free survival rate of 67%.9 The most common adverse events (≥ 20%) of any grade were headache, diarrhea, fatigue, and myalgia. Grade ≥ 3 hematologic toxicities (≥ 10%) included decreased neutrophils, decreased platelets, and decreased hemoglobin. These data led to U.S. Food and Drug Administration (FDA) accelerated approval of acalabrutinib for the treatment of adult patients with MCL following at least one prior line of therapy.10 Longer follow-up supported these results, with an estimated one-third of patients remaining progression-free at 36 months.11 Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
Zanubrutinib is a selective next-generation covalent BTK inhibitor with activity in B-cell malignancies, including relapsed/refractory MCL.12,13 In phase I/II trials in relapsed/refractory MCL (median of two prior lines of therapy), the overall response rate was 84.8% (62.5% complete response rate), with a median progression-free survival of 25.8 months and median overall survival of 38.2 months.14 The most common adverse events (≥ 30%), as reported in the pooled safety section of the U.S. prescribing information (USPI) for zanubrutinib, included decreased neutrophil count, upper respiratory tract infection, decreased platelet count, hemorrhage, and musculoskeletal pain.15 Grade 3 or 4 laboratory abnormalities (≥ 10%) consisted of decreased neutrophil count and lymphocytosis. Based on these data, zanubrutinib received FDA accelerated approval for the treatment of adult patients with MCL following at least one prior therapy, with continued approval for this indication contingent upon verification and description of clinical benefit in a confirmatory trial.
Both zanubrutinib and acalabrutinib are listed as preferred agents for second-line and subsequent therapy for MCL in current National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology (NCCN Guidelines®).16
Pirtobrutinib is a noncovalent, reversible BTK inhibitor that inhibits both wild-type and C481-mutant BTK at equally low nanomolar concentrations.8 Its higher specificity may result in less inhibition of off-target kinases than other BTK inhibitors, and its prolonged plasma half-life (~20 hours) allows for once-daily dosing.17 Pirtobrutinib was evaluated in the phase I/II BRUIN trial in patients with relapsed/refractory MCL who had received a median of three prior lines of therapy (including a BTK inhibitor). Results based on the primary analysis per protocol (which included phase I patients with a starting dose different from 200 mg) indicated an overall response rate of 58% (20% complete response rate); at a median response follow-up of 12 months, the median duration of response was 21.6 months.18 Data demonstrating the efficacy of pirtobrutinib (200 mg oral once daily) in heavily pretreated patients led to the FDA accelerated approval for the treatment of adult patients with relapsed/refractory MCL after at least two lines of systemic therapy, including a BTK inhibitor.19 This indication is approved under accelerated approval based on response rate; continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial. The approved prescribing information for pirtobrutinib includes an overall response rate of 50% (13% complete response rate), and a median duration of response of 8.3 months with 7.3-month median response follow-up.19 The most common adverse events (≥ 15%) in patients with MCL were fatigue, musculoskeletal pain, diarrhea, edema, dyspnea, pneumonia, and bruising. Grade 3 or 4 laboratory abnormalities (≥ 10%) were decreased neutrophil count, decreased lymphocyte count, and decreased platelet count.19 NCCN Guidelines® include pirtobrutinib as a treatment option for third-line or later therapy for relapsed/refractory MCL.16
Michael Wang, MD, Department of Lymphoma-Myeloma, The University of Texas MD Anderson Cancer Center, Houston, believes that “pirtobrutinib … will eventually bring about a paradigm shift in B-cell lymphoma.” Toby Eyre, MD, consultant hematologist at Oxford University Hospitals NHS Trust, added, “Pirtobrutinib may also be a treatment option for patients who are older or frailer and cannot tolerate or access CAR T-cell therapy.”
MCL becomes increasingly proliferative and aggressive over the course of the disease and throughout lines of therapy, so you really want to be thinking about risk and subsequent treatment options as early as possible. Toby Eyre, MD
Risk stratification in MCL is key, particularly prior to the use of a covalent BTK inhibitor. According to Dr. Eyre, high-risk patients with a TP53 mutation, high Ki-67 levels, and blastoid or pleomorphic morphology respond poorly to a covalent BTK inhibitor and have early disease progression. “MCL becomes increasingly proliferative and aggressive over the course of the disease and throughout lines of therapy, so you really want to be thinking about risk and subsequent treatment options as early as possible,” he emphasized.
CAR T-cell therapy targeting B-cell antigens such as CD19 has proven effective in various B-cell malignancies, including relapsed/refractory MCL.20 Dr. Wang indicated that CAR T-cell therapy is used in high-risk patients since responses with targeted therapies, including BTK inhibitors, often do not last very long in this patient population.
The CAR T-cell product brexucabtagene autoleucel was evaluated in the ZUMA-2 phase II trial in patients with relapsed/refractory MCL who had received at least two prior lines of therapy (including one or more BTK inhibitor). In the primary efficacy analysis, the overall response rate was 93% (67% complete response rate). The incidence of any-grade cytokine-release syndrome was 91% (15% grade ≥ 3), with 63% neurologic events of any grade (31% grade ≥ 3).21 At 3-year follow-up, the overall response rate was 91% (68% complete response rate), with a median progression-free survival of 25.8 months and median overall survival of 46.6 months. Durable responses were seen, including in patients with high-risk characteristics.22 These results led to accelerated approval of this agent for the treatment of relapsed/refractory MCL.23 Additional data support the efficacy observed in the pivotal trial.24,25 Brexucabtagene autoleucel is listed in NCCN Guidelines as a treatment option for relapsed/refractory MCL as third-line or later therapy, following chemoimmunotherapy and a BTK inhibitor.16
Lisocabtagene maraleucel is another CAR T-cell therapy approved for relapsed/refractory large B-cell lymphomas, although not specifically for MCL. In the TRANSCEND NHL 001 phase I trial, patients with relapsed/refractory large B-cell lymphoma who had received at least one prior line of therapy were infused with lisocabtagene maraleucel. In the relapsed/refractory MCL cohort (who had received a median of three prior lines of therapy), the overall response rate was 84% (59% complete response rate), with comparable efficacy noted in patients with high-risk features. Toxicities (any grade) included cytokine-release syndrome (54%) and neurologic events (28%), while the most common grade ≥ 3 treatment-emergent adverse events were neutropenia (41%), anemia (34%), and thrombocytopenia (31%).26,27 Updated data based on additional patients are anticipated.
To further improve efficacy, CAR T-cell therapy is being evaluated in combination with BTK inhibitors for relapsed/refractory MCL. Although trials vary according to the type of CAR T-cell product and BTK inhibitor used, encouraging activity has been seen, and studies are continuing.28
Adverse events related to BTK inhibitor therapy result from on-target effects as well as off-target inhibition of other kinases, with the frequency and severity of toxicities varying among approved agents.29 The need for long-term BTK inhibitor therapy increases the duration of drug exposure and risk of toxicities, so adverse event–related treatment interruptions and/or discontinuation may be required. For instance, a retrospective review found that discontinuations due to ibrutinib-related toxicity occurred in more than 25% of patients.30
Cytopenias are common with BTK inhibitors and may require a temporary dose hold or dose reduction if severe. The occurrence of neutropenia can increase the risk for infection. Clinicians should therefore monitor patients for infections, ensure that vaccinations are current, and consider Pneumocystis pneumonia prophylaxis for patients who are at increased risk.31 Dermatologic toxicities including bruising, ecchymosis, petechiae, changes in nails and hair, and skin opportunistic infections are also common, possibly due to off-target effects.32 Other BTK inhibitor–related toxicities such as fatigue, arthralgia, and headache are generally self-limited and considered manageable. Covalent BTK inhibitors can have class effects such as atrial fibrillation, bleeding, and infections. Dr. Wang noted that these adverse effects occur with pirtobrutinib, but most occurrences have been grade 1/2, even with protracted therapy. “But we need to remain vigilant,” he emphasized, “because so far we have used pirtobrutinib primarily in clinical trials.”
All BTK inhibitors pose a risk of cardiac events.33 Patient cardiac risk factors should be assessed when considering the use of BTK inhibitors, with cardiac monitoring during therapy. Clinicians should refer to published guidelines regarding the incidence and severity of adverse events with BTK inhibitor therapy, as well as recommendations on monitoring and management of common adverse events, including cardiovascular toxicities.34-36
While CAR-T-cell therapy can be effective, some toxicity is expected, so its use requires effective adverse event risk management. The main treatment-related adverse events include cytokine-release syndrome and immune effector cell-associated neurotoxicity syndrome (ICANS). Clinicians should be aware of currently used grading scales for cytokine-release syndrome and ICANS, as well as recommendations for management of these and other CAR T-cell–related adverse events.37 Other potential adverse events include cardiovascular, dermatologic, hematologic, gastrointestinal, and pulmonary toxicities. Neutropenia is common and can increase the risk of infections.38,39 Patients at high risk for cardiovascular toxicity should undergo careful cardiovascular risk assessment, with cardiac monitoring during therapy.40 A thorough clinical history is essential when considering CAR T-cell (or BTK inhibitor) therapy for relapsed/refractory MCL in order to identify patient comorbidities or increased risk of adverse events. Potential treatment-related toxicities should be discussed with patients when considering either treatment.
Emerging data suggest that a BTK inhibitor combined with various targeted therapies or immunotherapy may also be effective for relapsed/refractory MCL. For example, the combination of ibrutinib and venetoclax resulted in a 71% overall response rate and a median progression-free survival of 29 months.41,42 Newer-generation BTK inhibitors do not affect antibody-dependent cellular cytotoxicity, facilitating combinations of these agents with anti-CD20 monoclonal antibodies like obinutuzumab. There are ongoing trials evaluating the triplet combination of zanubrutinib, venetoclax, and obinutuzumab as well as acalabrutinib, venetoclax, and rituximab.43 Further research is needed to more fully evaluate these approaches for relapsed/refractory MCL, particularly as third-line or later therapy following prior BTK inhibitor treatment.
The advent of BTK inhibitors has had a significant impact on the treatment algorithm for relapsed/refractory MCL. Therapies such as noncovalent BTK inhibitors as well as CAR T-cell therapy are providing new treatment options for patients with relapsed/refractory MCL, particularly those with disease progression following two or more prior lines of therapy including a covalent BTK inhibitor. Toxicities associated with these treatments are generally manageable but require careful patient assessment for risk factors and monitoring during and after therapy for effective adverse event management. Ongoing studies are evaluating the optimal combinations and sequencing of these therapies to further improve outcomes for heavily pretreated patients with relapsed/refractory MCL.
Dr. Wang has received honoraria from Janssen Research & Development, Dava Oncology, OM Pharmaceutical Industries, AstraZeneca, CAHON, Hebei Cancer Prevention Federation, Mumbai Hematology Group, Acerta Pharma, Chinese Anti-Cancer Association, BeiGene, Clinical Care Options, Epizyme, Imedex, Kite, a Gilead company, Miltenyi Biomedicine, Moffit Cancer Center, Physicians' Education Resource, Breast-Gynecological International Cancer Society, Pharmacyclics/Janssen, Eastern Virginia Medical School, Leukemia & Lymphoma Society, LLC TS Oncology, Medscape, Meeting Minds Experts, OncLive/MJH Life Sciences, Practice Point Communications, First Hospital Zhejiang University, and BioInvent; has served as a consultant or advisor for AstraZeneca, Janssen Research & Development, Juno Therapeutics, Bioinvent, Pharmacyclics/Janssen, Loxo, Kite, a Gilead company, InnoCare, Oncternal Therapeutics, CStone Pharmaceuticals, Genentech, BeiGene, DTRM, Epizyme, Miltenyi Biomedicine, VelosBio, Deciphera, Juno Therapeutics, Lilly, and Pepromene; has received research funding from AstraZeneca, Janssen Research & Development, Pharmacyclics, Kite, a Gilead company, Juno Therapeutics, BeiGene, Acerta Pharma, Oncternal Therapeutics, Bioinvent, Loxo, VelosBio, Celgene, Molecular Templates, Lilly, InnoCare, Genmab, Genentech, and Vincerx Pharma; and reported travel, accommodations, and other expenses from Janssen Research & Development, AstraZeneca, Celgene, Dava Oncology, OM Pharmaceutical Industries, Kite, a Gilead company, and Physician Education Resources (PER).
Dr. Eyre has received honoraria from AbbVie, AstraZeneca/MedImmune, Autolus Therapeutics, Gilead Sciences, Incyte, Janssen Oncology, Loxo/Lilly, Roche, and Secura Bio; has served as a consultant or advisor for AbbVie, AstraZeneca/MedImmune, BeiGene, Incyte, Kite/Gilead, Loxo, Roche, and Secura Bio; and has received research funding from AstraZeneca/MedImmune and BeiGene.
VV-OTHR-US-DEL-1585 © 2023 Lilly USA, LLC. All rights reserved.
Sponsored content is not written by and does not necessarily reflect the views of ASCO or The ASCO Post editorial staff. It is authored by Harborside Studio writers or independent medical writers approved by Harborside Studio. Harborside Studio's sponsored content is held to editorial standards expected in The ASCO Post with the intent to provide valuable information to The ASCO Post readers. The mention of any company, product, service, or therapy does not constitute an endorsement of any kind by ASCO. ASCO assumes no responsibility for any injury or damage arising out of or related to use of the sponsored content or any errors or omissions. This sponsored content has been produced with funding support from Lilly. This sponsored content was developed under the direction and sponsorship of Lilly Medical Affairs and is intended for U.S. health-care professionals only.